Beyond the biological model of addiction
- jennagen
- Oct 26, 2021
- 5 min read
Updated: Dec 4, 2021

Addiction as a disease of the mind
In London Ontario, as in many medium to large size Canadian cities, there appears to be an increasing number of people who are injecting drugs. In 2014, more than 2.5 million needles were distributed in the community, making the needle distribution program the second largest in Canada after Vancouver’s (Campenella, 2015, August 14). The increasing number of people who inject drugs seems to infer that past treatment models have not been successful. Perhaps there is a more effective way of viewing and treating addiction.

Biological models of addiction emphasize the importance of genetics and the biological forces of nature. These theories suggest that brain chemistry, brain structure, and genetic abnormalities cause human behavior (American Addiction Centers, 2021). While the biological models of addiction have been helpful in decreasing stigma surrounding drug use, these models fail to recognize there are social determinants of health that are highly correlated with illicit drug use.

Multilevel understanding of addiction
In health care we are beginning to understand that many factors influence health outcomes. One does not become a person who injects drugs based on genetics alone. Multilevel models of health expand beyond the individual/genetic factors in disease processes and acknowledge that environment, education level, socio economic status, political environment, and culture have consequences on an individuals health status. A multilevel approach to population health is predicated on the understanding that exposures at many levels of organization work together to produce health outcomes. These exposures are positioned both up and downstream of individual-level risk factors and include determinants of population health that are social, biological, geographic, political, and temporal in nature (Galea, 2015).
The biopsychosocial model
The biopsychosocial model is a reaction to the biological model of addiction popularized in the 1960’s. This model was proposed by Engels in 1977 and suggests that health and well-being can only be understood by looking at the intersection of biological, psychological, and social factors.
The biopsychosocial model of addiction (Becona,2018) states that genetic/biological, psychological, and sociocultural factors contribute to substance consumption and should be taken into account for prevention and treatment. Becona’s article is particularly interesting as it further illustrates divergence from the biological model of addiction.
The article references a classic study where a sample of Vietnam veterans who tested positive for opiates were followed upon their return to the United States. Of the general sample, 43% had used narcotics in Vietnam, 34% had used heroin, and 20% were addicted to narcotics. Between 8 and 12 months after returning home, only 10% had used narcotics, and the number of those addicted to heroin decreased to 1%. The article argues the onset of drug consumption is not biological, but social. If the biological model of addiction were a truism, many Vietnam veterans would have remained addicted to opiates, or required extensive rehabilitation supports.
The biopsychosocial model of health: Microsystem

Source: Physio-pedia https://www.physio-pedia.com/Biopsychosocial_Model
The biopsychosocial model of health microsystem suggests the individual’s mental health is influenced by such factors as; social: peers, family circumstances; psychological: self-esteem, coping skills, social skills; biological: physical health, disability and genetic vulnerabilities. These spheres overlap and are influenced by: family relationships, trauma, temperament, IQ, and drug effects.

Is there a social/psychological factor that may influence illicit drug use?
Research demonstrates a strong link between exposure to traumatic events and substance use problems. Many people who have experienced child abuse, criminal attack, disasters, war, or other traumatic events turn to alcohol or drugs to help them deal with emotional pain, bad memories, poor sleep, guilt, shame, anxiety, or terror (International Society for Traumatic Stress Studies, n.d.). Understanding trauma as a factor in illicit drug use is an important step when designing and providing treatment and support programs.
The biopsychosocial model of treatment: beyond the individual
Below is an infographic which illustrates the exosystem and macrosystem in which each individual who injects drugs is centered.
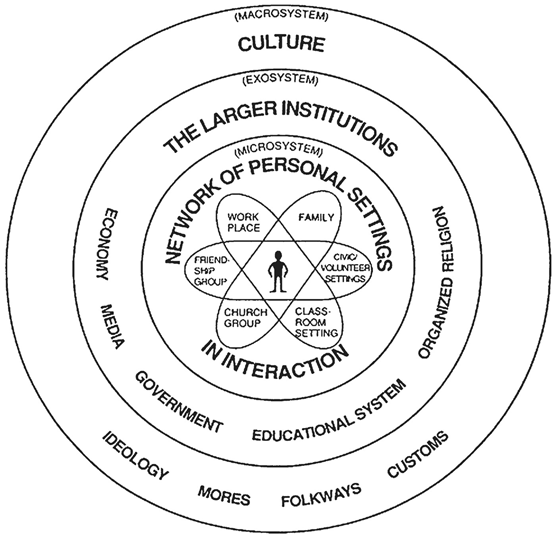
Bronfenbrenner’s Bioecological Theory. Source: https://doi.org/ 10.1111/spc3.12328B
How does the exosystem impact people who inject drugs?
In the biopsychosocial model, the government and the polices it adopts, is part of the exosystem. The government is responsible for social engineering and public policy approaches to substance-related problems have had some success, adding further support to the biopsychosocial model of addiction. For example, when alcohol was made illegal during prohibition, national rates of drinking and associated health consequences such as cirrhosis of the liver were reduced (Skewes, & Gonzalez, 2013).
In the population of people who inject drugs it does not appear that prohibition is working to reduce negative outcomes. Perhaps the government needs to move away from outdated ideas of prohibition and adopt a biopsychosocial model of treatment that supports illicit drug users in dealing with trauma.

Trauma informed approach to treatment
The Centers for Disease Control and Prevention (CDC), Office of Public Health Preparedness and Response (OPHPR), in collaboration with SAMHSA’s National Center for Trauma-Informed Care (NCTIC) (2020), developed and led a new training for OPHPR employees about the role of trauma-informed care during public health emergencies. I argue the opioid crisis is a public health emergency which warrants a trauma informed approach to treatment.
What are the 6 guiding principles to a trauma informed approach?
Safety
Trustworthiness & transparency
Peer support
Collaboration & mutuality
Empowerment & choice
Cultural, historical & gender issues

Future Focus
By creating addiction treatment programs with the 6 guiding principles of a trauma informed approach, our society will be moving away from the biological model of addiction toward a more holistic biopsychosocial model of care. Employing the biopsychosocial model of addiction acknowledges that while genetics influence individual health outcomes, there are many other factors that act on the individual as well. By taking the focus off genetics, and placing it on factors that can be modified and improved perhaps individuals can benefit from improved outcomes.
References
American Addiction Centers. (2021). Biological causes of addiction. Retrieved from https://www.mentalhelp.net/addiction/biological-causes/
Becoña, E. (2018). Brain disease or biopsychosocial model in addiction? Remembering the Vietnam Veteran Study. Psicothema, 30(3), 270-275. Retrieved from http://www.psicothema.com/pdf/4481.pdf
Campanella, E. (2015, August 14). More than 2.5 million needles distributed in London last year. London Free Press. Retrieved from https://lfpress.com/2015/08/13/more-than-25-million-needles-distributed-in-london-last-year
Centers for Disease Control and Prevention. (2020, September 17). Infographic: 6 guiding principles to a trauma-informed approach. Retrieved from https://www.cdc.gov/cpr/infographics/6_principles_trauma_info.htm
Galea, S. (2015, May 31). The determination of health across the life course and across levels of influence. Boston University School of Public Health. Retrieved from The Determination of Health Across the Life Course and Across Levels of Influence | SPH (bu.edu)
International Society for Traumatic Stress Studies. (n.d.). Traumatic stress and substance abuse problems. Retrieved from https://istss.org/ISTSS_Main/media/Documents/ISTSS_TraumaStressandSubstanceAbuseProb_English_FNL.pdf
Lehman B.J., David D.M., Gruber J.A. (2017). Rethinking the biopsychosocial model of health: Understanding health as a dynamic system. Soc Personal Psychol Compass. https://doi.org/ 10.1111/spc3.12328B
Physio-pedia. (2021). Biopsychosocial model. Retrieved from https://www.physio-pedia.com/Biopsychosocial_Model
Scheim, A., Rachlis, B., Bardwell, G., Mitra, S., & Kerr, T. (2017, April 11). Public drug injecting in London, Ontario: a cross-sectional survey. CMAJ. 5(2), E290-E294. Retrieved from https://www.cmajopen.ca/content/5/2/E290#ref-16
Skewes, M., & Gonzalez, V. (2013). The biopsychosocial model of addiction. Principles of addiction. 61-70. Retrieved from https://books.google.ca/books?hl=en&lr=&id=5gRNl3oIwWEC&oi=fnd&pg=PA61&dq=biopsychosocial+model+of+addiction&ots=j7Oo92Yfqv&sig=e5TYD2vS4Ua6dKYeoPMOkRp8nk4#v=onepage&q=biopsychosocial%20model%20of%20addiction&f=false



Comments